While the world marks UN-designated World Sickle Cell Day on 19 June, global health system Cleveland Clinic is making great strides in a clinical trial to evaluate the use of gene-editing therapy as a potential cure for the disease. According to the lead investigator of the clinical trial, this is one of several significant recent developments that can benefit patients with the inherited blood disorder.
Rabi Hanna, M.D., a pediatric hematologist-oncologist at Cleveland Clinic Children’s, says, “This is an exciting time in the field of sickle cell disease, with the advances in research and development of new therapies offering real hope to patients. Sickle cell disease can severely impact on patients’ quality of life and limit their potential due to the extreme pain episodes, end-organ damage, and reduced life expectancy. Medications can modify disease severity and treat symptoms, but the average life of a sickle cell patient is in the mid-40s, which is why it is important for us to find a cure.”
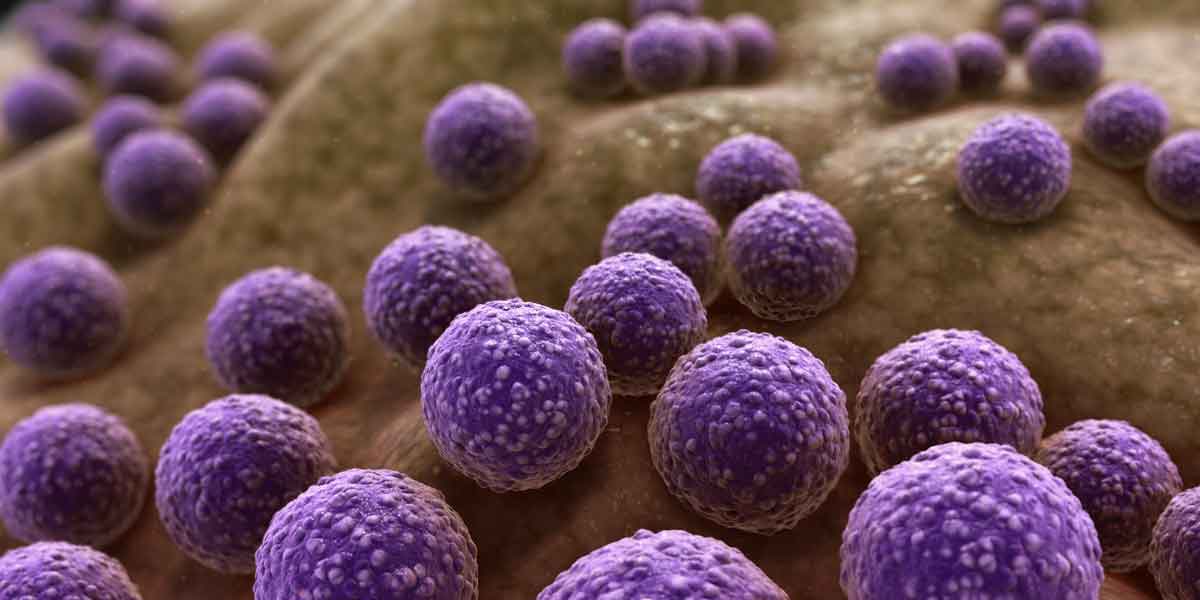
In people with the disease, a genetic change in DNA causes a chemical alteration in hemoglobin — a red protein responsible for transporting oxygen in the blood — resulting in cells becoming sickle shaped, rather than round. The sickle-shaped cells do not pass easily through blood vessels, and can clog or break apart, leading to decreased red blood cell life and increased iron storage in the liver and heart. This can cause conditions such as liver fibrosis, liver failure, stroke, cardiomyopathy and heart failure along with severe pain.
Dr. Hanna explains that although sickle cell disease was discovered as early as 1910, there was little research or progress in its treatment until recent decades. From the 1990s onwards, a blood or marrow transplant began to be offered as a cure for select sickle cell disease patients, but it could be challenging to find a matched donor and there were significant risks involved. In the past 10 years, the potential donor pool for patients has been expanded due to new procedures for haplo-identical transplants pioneered by centers such as Cleveland Clinic, but the significant risks remain a problem.
Explaining the risks, Dr. Hanna says, “First, there is a 5% to 10% risk of your body rejecting the donor cells. Second, there is the risk of severe graft-versus-host disease, which occurs when donor bone marrow or stem cells attack the recipient. To prevent this, the patient is given strong immunosuppressant drugs, but there is still a significant risk of graft-versus-host disease.”
In contrast, gene therapy uses the patient’s own stem cells and, therefore, the risks of rejection or graft-versus-host disease are eliminated, Dr. Hanna explains. Another benefit of gene therapy is that patients will not need immunosuppressant drugs so their immune systems will function normally, which is particularly important during a pandemic, he says. In addition, while patients need chemotherapy to prepare the body in both traditional transplants and gene therapy, the chemotherapy used in gene therapy is less strong.
Describing the procedure, Dr. Hanna says, “Gene therapy is a ground-breaking technology that works by replacing or inactivating disease-causing genes. In our clinical trial, we are introducing healthy genes into the body with the goal of correcting genetic abnormalities of red blood cells. By enabling the cells to produce more fetal hemoglobin, this treatment has the potential to cure sickle cell disease in a precise way.”
During the study, patients’ stem cells are collected for gene editing in a laboratory. Patients are then treated with chemotherapy to destroy the remaining bone marrow to make room for the repaired cells that are infused back into the body. The patients will undergo the treatment at different times and will be monitored closely afterwards for up to two years to see if there are any long-term side effects before the trial results are released.
In the meantime, however, patients living with sickle cell disease are benefiting from other recent research that has led to the introduction of newer medications for the first time after many years, says Dr. Hanna. The medications, which were approved by the US Food and Drug Administration (FDA) in 2019 and 2021 respectively, are crizanlizumab to reduce severe pain and complications, and voxelotor to help restore normal red blood cell function and oxygen delivery to tissues and which also helps with pain.
“For patients and the medical community, there is a lot to be optimistic about on this year’s World Sickle Cell Day. After little progress in treatment methods during the last century, the disease is now being given the attention it deserves and all of the current research projects underway are set to make a real difference in patients’ lives,’ concludes Dr. Hanna.
According to the World Health Organization, approximately 5% of the world’s population carries trait genes for hemoglobin disorders, mainly, sickle-cell disease and thalassemia. It should be noted, however, that this does not mean they will develop the disease. It is estimated that 300,000 babies with severe hemoglobin disorders are born each year. India and countries in the Middle East and Africa are among those with a higher prevalence for sickle cell disease.