With the availability of vaccines against human papillomavirus (HPV) and the ability to remove abnormal cells before cancerous lesions develop, cervical cancer could become a disease of the past for future generations, says an expert from global health system Cleveland Clinic, speaking during the Cervical Cancer Awareness Month of January.
Cervical Cancer is the fourth-most common cancer among women worldwide and is caused mainly by persistent infection with high-risk types of HPV, according to the World Health Organization (WHO). In its recent publications, the WHO estimates there were 604,000 new cases and 342,000 deaths from cervical cancer in 2020.
“The good news is that cervical cancer is preventable, and also highly treatable, especially if caught early,” says consultant gynaecological-oncology surgeon Owen Heath MBBS MRCOG PhD, who practises at Cleveland Clinic London.
According to Dr. Heath, a combination of HPV vaccines and regular screening are needed to eliminate cervical cancer. “While studies in the UK and Australia have highlighted the effectiveness of HPV vaccine programs in reducing the incidence of cervical cancers and pre-cancers, more research is needed,” he says. “Regular screenings remain vital as some people may elect not to have the vaccine, or in some countries the vaccine might not cover all of the high-risk HPV types. In extremely rare cases, a cervical cancer could develop that is not directly linked to HPV.”
The vaccines are normally administered to school children and in adults up to the age of 45, after which the likelihood of developing cancer from HPV is lower, although regular cervical cancer screenings should continue. Dr. Heath points out that the vaccines are not just for women, in addition to transmitting the disease, men are also at risk of other health issues caused by strains of the HPV such as head and neck cancers.
Dr. Heath says cervical cancer can develop slowly with pre-cancerous cells becoming cancerous over a period of many years, so regular screening is important. While guidelines vary from country to country, he recommends women visit a doctor to ask about the screening frequency needed based on their individual risk profile. According to Dr. Heath, women above the age 65 can discontinue screening if this has been previously normal, but since cervical cancer can develop at any age, it is important to see an expert if there are any gynaecological symptoms.
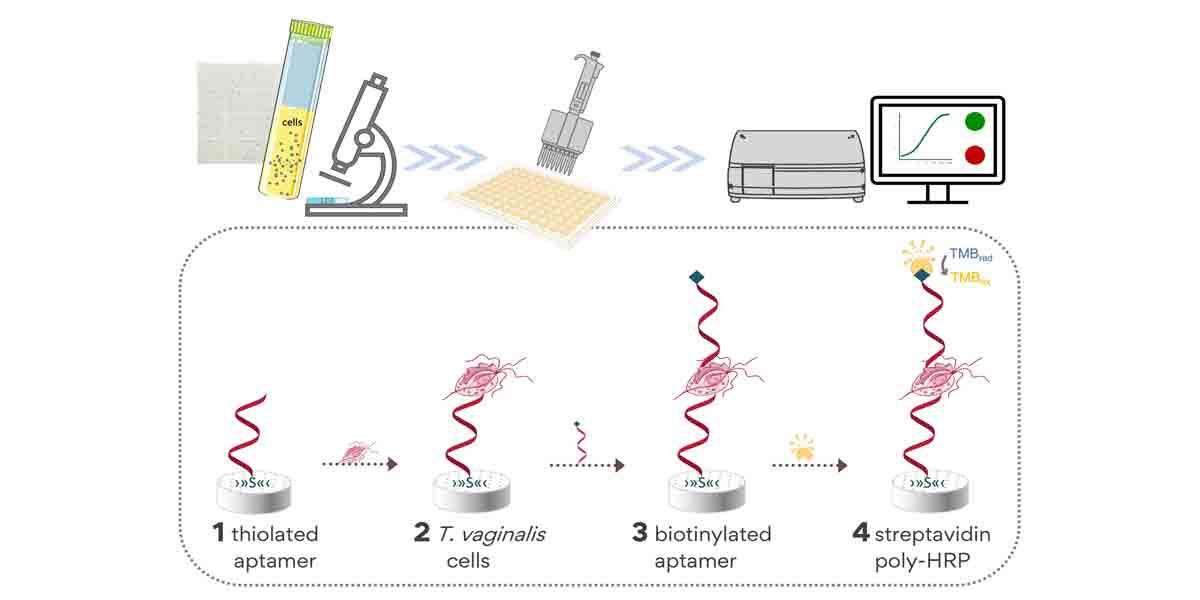
The most common screening test now combines HPV testing with a pap smear. A cervical sample is analysed for the presence of high-risk HPV subtypes, if high-risk HPV subtypes are detected the cells in the sample are then looked at for any abnormalities, Dr. Heath adds.
If a high-risk form of HPV is found in a woman, she will need to be monitored carefully, typically through annual screening. “In the majority of cases, the body’s own immune system can clear the infection, but if it persists it can cause abnormalities in the cells of the cervix that left untreated can develop into a cervical cancer. If there is evidence of persistence of HPV infection or cytological abnormalities, a detailed examination of the cervix called a colposcopy should be undertaken. This is a quick and effective means to achieve a diagnosis. Treatment of pre-cancerous areas on the cervix can be undertaken at the same time, by removing or ablating these cells,” says Dr. Heath.
If a patient is diagnosed with cervical cancer, surgical removal of the cancerous tissue is very successful if the cancer is detected at an early stage, says Dr. Heath. He adds that fertility-preserving procedures could be offered at this stage, for example, a trachelectomy, where the cervix is removed but the womb remains. Later-stage cancers are treated with the combination of radiation and chemotherapy.