By Francis Allan L. Angelo
Oral nicotine pouches (ONPs), sleek, discreet, and often flavored, are rapidly gaining traction in the US market, especially among young adults.
Marketed as “tobacco-free,” these pouches deliver nicotine via the oral mucosa, bypassing the combustion associated with traditional tobacco products like cigarettes.
While preliminary research suggests that ONPs may present fewer health risks than conventional alternatives, experts are urging caution and emphasizing the urgent need for independent scientific investigation to inform regulation and protect public health.
The allure of flavors, coupled with aggressive marketing tactics that emphasize convenience and discreet use, has sparked concerns about ONPs’ potential to attract a new generation of nicotine users.
These worries are not unfounded, considering the parallels with the trajectory of e-cigarettes, which initially gained popularity among smokers seeking harm reduction but subsequently fueled a surge in youth nicotine addiction.
A recent cross-sectional survey of 118 adult ONP users in the US, published in Nicotine and Tobacco Research, revealed that the availability of preferred flavors was the most cited motivation for using these products.
Mint and tobacco flavors emerged as favorites, with Zyn and Lucy dominating brand preferences. The study also found significant levels of dependence among participants, indicating the potential for ONPs to be addictive.
Moreover, nearly half of the respondents reported experiencing adverse events, primarily mouth lesions and gastrointestinal issues.
However, the study’s authors acknowledge the limitations of their findings, particularly the small and homogeneous sample size, urging larger, more diverse studies to confirm these results.
This call for broader research is echoed in a comprehensive review published in Experimental and Clinical Psychopharmacology, which synthesizes the available scientific evidence on ONPs.
This review underscores the dramatic growth of the ONP market and the critical need for robust, independent research to guide regulatory decisions. While the review acknowledges the potential for ONPs to offer a less harmful alternative to conventional tobacco products for individuals who fully switch, it flags several key areas of concern:
-The dearth of independent research: The vast majority of clinical studies on ONPs have been funded by the tobacco industry, raising concerns about potential bias and the need for objective, academically driven investigations.
-The allure for youth and young adults: ONPs’ attractive flavors, discreet usability, and “tobacco-free” marketing claims mirror the tactics that propelled youth e-cigarette use.
-The need for long-term studies: The long-term health effects of ONP use are still largely unknown. Longitudinal studies are necessary to determine whether ONPs lead to the adoption of more harmful products among non-users and whether they effectively facilitate a complete transition away from conventional products among existing users.
These concerns were further highlighted during a recent expert briefing held by the Johns Hopkins Bloomberg School of Public Health, featuring insights from Dr. Joanna Cohen, Bloomberg Professor of Disease Prevention and Director of the Institute for Global Tobacco Control, and Dr. Johannes Thrul, Associate Professor in the Department of Mental Health.
Dr. Cohen emphasized the importance of comprehensive, evidence-based regulation for ONPs, particularly in addressing marketing practices, youth access, and transparency about potential health risks.
Dr. Thrul echoed these sentiments, adding that while ONPs may hold promise as harm reduction tools, “the benefits must be weighed carefully against the risks of increasing nicotine use among youth and consumers who don’t already smoke.”
The experts also addressed the broader landscape of tobacco control, acknowledging global progress in reducing cigarette smoking but cautioning against complacency in the face of evolving industry tactics.
Dr. Cohen expressed concern about the industry’s tendency to “exploit any loopholes that they can find to undermine the spirit of the law,” particularly in relation to novel products like ONPs.
The briefing also touched upon the debate surrounding e-cigarettes, with both experts stressing the need for clear messaging about their inherent health risks, despite the industry’s push to frame them as harm reduction tools.
While some clinical trials suggest that e-cigarettes can assist smoking cessation, real-world data paint a more complex picture, with concerns about dual use hindering complete nicotine abstinence.
Moreover, Dr. Thrul highlighted the lack of a comprehensive understanding of the health effects of nicotine in isolation, particularly in the context of novel delivery mechanisms like ONPs. This knowledge gap underscores the need for research that goes beyond industry-funded studies, particularly in investigating long-term health outcomes.
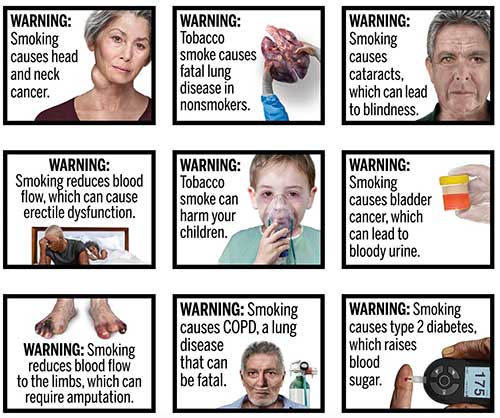
Dr. Cohen also expressed disappointment with the persistent delays in implementing graphic warning labels on cigarette packs in the US, attributing the holdup directly to the tobacco industry.
Despite evidence from other countries showing the effectiveness of graphic warnings in reducing smoking initiation, particularly among youth, the US lags behind, highlighting the industry’s influence in thwarting evidence-based policies.
In addressing the potential for stricter regulation to fuel a black market for tobacco products, Dr. Thrul argued that fears of widespread illicit trade are often exaggerated by the industry.
Evidence from other countries suggests that robust enforcement and monitoring, coupled with public education, are more effective in mitigating illicit markets than resisting regulation altogether.
The expert briefing also discussed heated tobacco products, which heat tobacco instead of burning it to generate an inhalable aerosol containing nicotine.
While these products may expose users to lower levels of harmful chemicals than traditional cigarettes, they are not risk-free. More research is needed to fully evaluate their short- and long-term health effects.
Finally, the experts stressed the crucial role of healthcare professionals in supporting patients seeking to quit tobacco products, emphasizing the effectiveness of brief advice, referrals to cessation resources, and prescription of FDA-approved medications when appropriate.
In conclusion, the emergence of ONPs presents a complex challenge for public health. While the potential exists for these products to serve as less harmful alternatives for established tobacco users seeking to completely switch, the limited available evidence, dominated by industry-funded research, warrants cautious optimism.
The parallels with the trajectory of e-cigarettes, particularly concerns regarding youth appeal and the long-term health consequences of nicotine use, underscore the need for vigilance and proactive measures.
Robust, independent research is urgently needed to inform effective regulations that prioritize public health and prevent ONPs from becoming another gateway to nicotine addiction, especially for vulnerable populations like youth.
















